If you are a caregiver for someone who is bedridden, uses a wheelchair, or has limited mobility, understanding bedsores(also known as pressure ulcers or pressure injuries) is critical. These sores are more than a minor skin issue—they are a serious medical condition that can lead to severe complications if ignored. The key to prevention is early detection.
In this article, we answer two vital questions:
What are the early warning signs of a bedsore? and
How long does it take to get a bedsore?
How Fast Can a Bedsore Form? (The Timeline Might Shock You)
Many people are shocked to learn just how quickly a bedsore can begin to form.
The initial damage can start in as little as 2 to 3 hours of uninterrupted pressure.
To understand why, try this simple experiment: lean your elbow on a hard table and put your full weight on it.
•Within a few minutes, it becomes uncomfortable.
•After 15 minutes, it becomes painful.
•Now, imagine you cannot move away from that pain. The tissue becomes starved of blood flow, and the area goes numb. After just a few hours, the skin and tissue are damaged.
This is why the standard of care is to reposition immobile individuals every 2 hours. For someone in a wheelchair, small weight shifts are needed every 15 to 30 minutes. This simple action is the most effective way to prevent pressure sores.
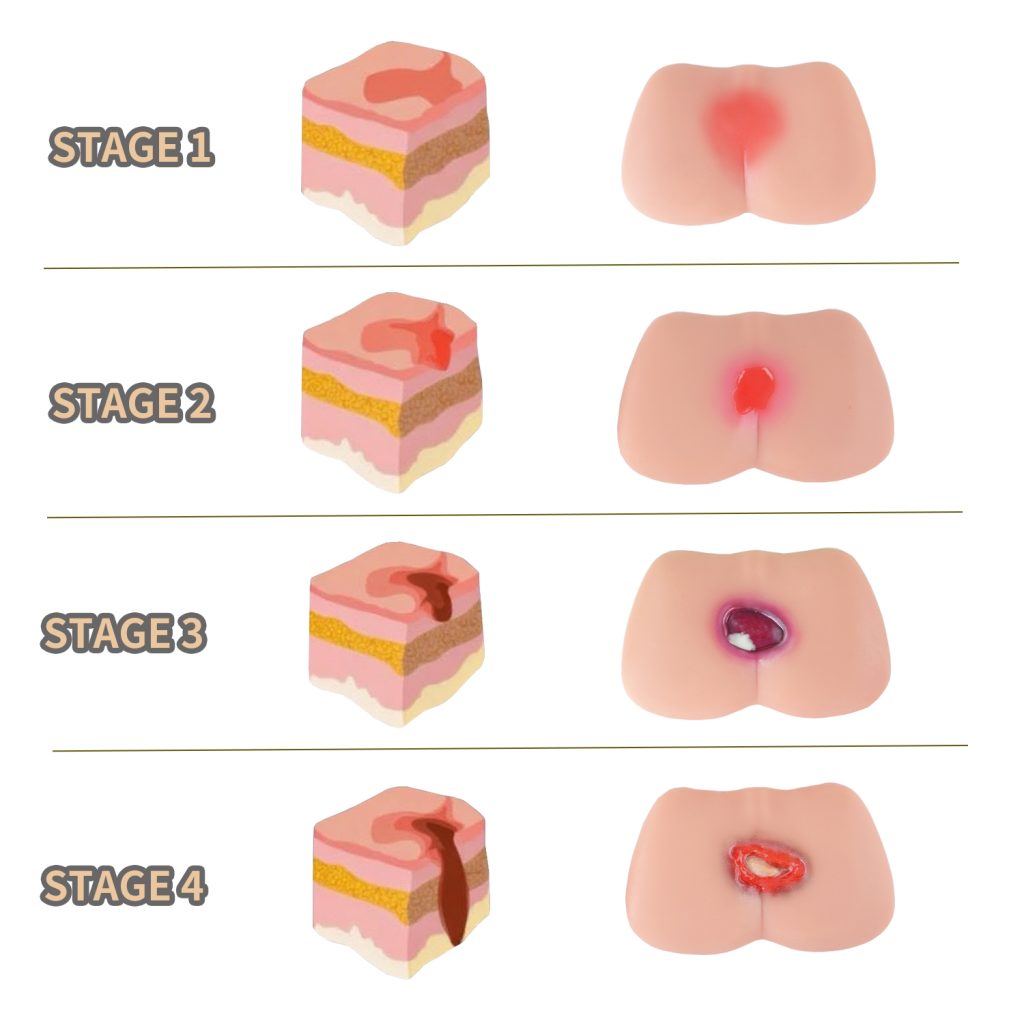
Early Warning Signs of Bedsores (Stage 1 Pressure Ulcer Symptoms)
Catching a bedsore at its earliest stage (known as a Stage 1 pressure ulcer) is the key to preventing a more severe wound. Before a visible sore appears, your body sends signals. Check bony areas daily—heels, tailbone (coccyx), hips, ankles, and shoulder blades—for these signs:
1. Unusual Skin Discoloration:
This is the most common early sign.
•On lighter skin: Look for a persistent red patch that does not turn white when you press it (this is called non-blanchable erythema).
•On darker skin: The patch may appear blue, purple, or ashen (darker than the surrounding skin). The area may also feel warm and look shiny.
2. Changes in Skin Temperature or Texture:
•The area may feel noticeably warmer or cooler than the skin around it.
•The skin may feel unusually firm(hard) or soft (mushy).
3.Pain or Sensation:
•The person may complain of pain, itching, or a burning sensation in a specific spot.
•For those who cannot communicate, watch for signs of discomfort like grimacing, moaning, or pulling away when the area is touched.
Immediate Action:
If you see any of these early warning signs, relieve all pressure from that area immediately. Do not massage the reddened zone, as this can cause further tissue damage.
Who Is Most at Risk for Developing Bedsores?
While anyone with limited mobility can develop a pressure injury, some factors significantly increase the risk:
•Complete immobility(e.g., spinal cord injuries, advanced dementia, paralysis).
•Being underweight or malnourished, with less fatty tissue to cushion bones.
•Previous history of pressure sores.
•Health conditions that affect blood flow, like diabetes or vascular disease.
•Skin moisture from incontinence or sweat, which makes skin more fragile.
How to Prevent Bedsores: Turning & Repositioning Tips
Prevention is always better than treatment. Here’s how you can protect your loved one:
•Strict Repositioning Schedule:
•Change positions in bed at least every 2 hours. Use a schedule chart as a reminder.
•Use Support Surfaces: Invest in a pressure-relieving mattress(or alternating air mattress) or specialized cushions for wheelchairs and chairs.
•Perform Daily Skin Checks: Make a quick head-to-toe skin inspection part of your daily routine.
•Ensure Proper Nutrition and Hydration: Healthy skin is more resilient. Enough protein, calories, vitamins (especially Vitamin C and Zinc), and water are essential for skin health.
•Manage Moisture: Keep skin clean and dry. Use moisture-wicking bedding and change clothes and sheets promptly if they become damp.
Conclusion: Vigilance Prevents Pain
The timeline for a bedsore is alarmingly fast, but your power to prevent it is immense. By understanding the early signs of a pressure ulcer and committing to a consistent routine of turning and repositioning, you are the first and most important line of defense.
Always document any skin changes and consult a healthcare professional or wound care specialist immediately if you suspect a bedsore is forming. Early action can prevent weeks of pain and complex treatment.
